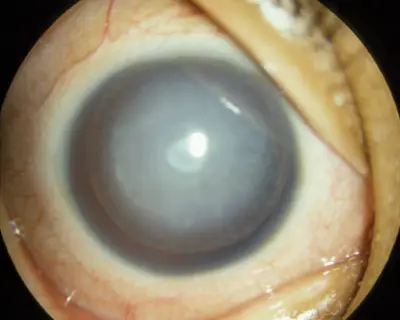
A cataract is any cloudiness or opacity of the natural lens of the eye, which is normally crystal clear. An eye’s lens must be clear to focus the images it sees onto the retina, which then sends the images to the brain. A cataract can prevent light from reaching the retina. It can also cause light rays to scatter as they pass through the cloudiness. Cataracts are a common and frequently curable cause of blindness in children. Early detection and prompt intervention are critical for a good visual outcome, particularly in newborns.
The reported prevalence of childhood cataracts ranges from 1 to 15 per 10,000 children. Untreated cataracts in children lead to tremendous social, economic, and emotional burdens to the child, family, and society. They can affect one eye (unilateral) or both eyes (bilateral). Some cataracts are small and don’t cause any trouble with vision. Other more progressive cataracts can cause visual problems in children.
Causes of Pediatric Cataracts
Cataracts in a child can be congenital (present at birth) or acquired (develop after birth). Also, some pediatric cataracts may actually be congenital cataracts that simply weren’t identified earlier because the child did not have his or her first eye exam until they were older.
Most unilateral and a significant number of bilateral cataracts are idiopathic in nature. The diagnosis of such cases is made after excluding other causes.
Approximately 50% of childhood cataracts are caused by mutations in genes that code for proteins involved in lens structure or clarity. Metabolic disorders can cause cataracts, which may have particular morphologies that point to the underlying cause.
Congenital infections such as Toxoplasma, rubella, cytomegalovirus, herpes, and syphilis (TORCH) are associated with congenital cataracts, with rubella being the most common.
Other causes of childhood cataracts in older children include trauma, drug-induced, radiation, uveitis, intraocular tumours and laser therapy for retinopathy of prematurity. Trauma is one of the commonest causes of unilateral cataracts in developing countries.
Bilateral cataracts occur commonly due to the long-term use of topical or systemic steroids.
Morphology
The human crystalline lens consists of three parts including a center part (nucleus), an outer part (cortex) and a capsule surrounding the cortex. Cloudiness can occur in one or more parts of the lens:
- A lamellar cataract is a cloudiness between the nuclear and cortical layers of the lens.
- A nuclear cataract is a cloudiness of the center part of the lens.
- A posterior subcapsular cataract is a thin layer of cloudiness that affects the back surface of the lens cortex, just inside the capsule. This type of cataract can often be associated with medication use such as steroids.
- An anterior polar cataract is a small, usually central opacity of the front part of the lens capsule. Anterior polar cataracts generally do not grow during childhood and are typically not visually significant. They are often managed without surgery.
- A posterior polar cataract is a central opacity at the back of the lens.
- Persistent fetal vasculature can be associated with pediatric cataracts. During the development of the eye, a blood vessel extends from the optic nerve (in the back of the eye) to the developing lens to provide nutrients to the young, growing lens. This blood vessel normally disappears before birth. If the blood vessels do not go away, it can result in a plaque-like cataract on the back of the lens. The persistent stalk extending from the back of the eye toward the cataract can cause retinal abnormalities as well.
- A traumatic cataract results from either a blunt or penetrating force that damages the lens. The cataract can form shortly after the trauma or months to years after the injury
Symptoms of Pediatric Cataract
- A pupil that looks white when a flashlight is shined into it
- Eyes that aren’t in the right position (misaligned)
- Rhythmic eye movements that can’t be controlled (called nystagmus). The eyes may go back and forth, up and down, around, or mixed.
- Cloudy or blurry vision
Children’s eyes and brain are still learning to see. This is why distortion can lead to lazy eye or amblyopia in children.
Evaluation
Vision screening is mandatory to detect cataracts as soon as possible. Late detection may result in poor visual outcomes. All newborns must have red reflex screening, ideally followed by another red reflex examination at the 6-8 week neonatal checkup.
A detailed history is taken that includes asking about the child’s developmental milestones, and about health problems in the siblings and parents.
Leukocoria (white reflex) is often noticed by family members as a finding in the eye of the child. However, every white reflex is not a cataract. Retinoblastoma is the most serious and a common cause of white reflex in the child. Other pathologies which may present with white reflex in the eye should be ruled out.
Visual assessment should be performed using patterns of fixation and supplemented when possible by preferential looking charts or pattern visual evoked potentials.
Measurement of corneal diameter, intraocular pressure, pupillary reflexes, and indirect ophthalmoscopy should be carried out. Ultrasonography (USG) helps us rule out retinal detachment, fundal coloboma, and retinoblastoma. USG in a case of unilateral cataract can diagnose a PFV.
In unilateral cases and in an otherwise healthy infant with one parent involved by the disease, an extensive preoperative investigation is not necessary to establish the cause for cataract.
If there is no family history of cataracts, a pediatric systemic evaluation is required because these cataracts may be associated with systemic or metabolic disease.
A urine test for reducing sugars, TORCH (toxoplasmosis, rubella, cytomegalovirus, varicella) screening, a Venereal Disease Research Laboratory (VDRL) test for syphilis, and a blood test for calcium, phosphorus, glucose, and galactokinase levels can be checked.
Timing of surgery
The critical period of eye development ranges from 2 months to 6 months of age. Surgery is advised in visually significant opacities, i.e. more than 3-mm central opacity.
Unilateral cataracts should be operated as early as possible before 6 weeks of age and bilateral cataracts should be operated before 8 weeks of age. In symmetric cataracts, the second eye is operated within 1 week of the first eye and in a systemically unstable child it can be performed in the same sitting. A delay in cataract removal can interfere with normal development of the vision centers in the brain.
In visually nonsignificant opacities (blue-dot cataract or small posterior polar), the child can be observed at regular intervals.
Pediatric Cataract Surgery
Surgical removal of a cataract in an infant or child is done under general anesthesia using an operating microscope. Examination under anesthesia is carried out to record the essential parameters for intraocular lens (IOL) power calculation.
The very soft and cloudy inner part of the child’s lens is suctioned out of the capsule. Younger children may require an additional opening in the posterior lens capsule with some vitreous gel removal (called a vitrectomy). Dissolvable stitches are used to close the wounds.
Once the cataract has been removed, focusing power may be restored in one of the following ways:
- Intraocular lenses: artificial lenses may also be implanted to replace natural lenses in children. An intraocular lens (IOL) is then sometimes placed within the empty lens capsule either during the same surgery or in a subsequent second surgery. Generally, an IOL is not placed in a patient less than 1 year of age. Intraocular lenses have the potential to reduce the magnification and optical distortion often associated with other methods of restoring focusing power, such as glasses. Intraocular lenses are permanent replacements for the natural lens and, therefore, require less maintenance than contact lenses.
- Contact lenses: used after surgery for bilateral or unilateral cataracts in children under 2 years of age. A contact lens can be placed on the surface of the eye (contact lenses have to be removed and cleaned regularly)
- Glasses: used in selected cases when the cataract surgery involves both eyes and contact lenses have failed, or if intraocular lenses are not appropriate. Once the cataract is removed, glasses are often very thick and cause magnification, so they are generally not a good option when only one eye is affected. They can also limit the visual field of the affected eye.
Postoperatively, a child’s eye tends to show more tissue reaction. The inflammatory response can be managed with the use of intensive topical steroid (as frequently as six to eight times a day). The steroids are tapered over a period of 6 to 8 weeks.
Topical antibiotics are instilled three times a day for 10 to 14 days.
Homatropine eye drops (2%) twice a day or atropine eye ointment once a day should be used for about four weeks to prevent posterior synechiae formation.
Refraction should be done as soon as inflammation subsides and appropriate correction should be provided based on the age of the child.
The final step in the treatment process is to treat amblyopia which develops if one eye is stronger than the other, as in the case of a unilateral cataract. In patients with unilateral or asymmetric cataracts (one cataract is more severe than the other), it is necessary to patch the good eye to stimulate vision in the eye that had the cataract surgery. All patients who undergo cataract surgery also require bifocal glasses to correct the residual error of refraction and to allow focusing at a distance and near.
Complications of Cataract Surgery
- Cataract surgery performed by an experienced surgeon is generally very safe. However, no surgical procedure is without risks.
- Posterior capsular opacification is the most common complication after cataract surgery with or without IOL surgery in children. In a thick PCO, surgical posterior capsulotomy is required to prevent amblyopia. Nd: YAG laser is a noninvasive option in older children for PCO.
- Glaucoma following cataract surgery is observed in 10%–25% of children. Younger age at surgery and the presence of microphthalmia are high-risk factors. Intraocular pressure may be controlled on medication or may require surgical intervention.
- Postoperative uveitis (fibrinous or exudative) is a common complication due to increased tissue reactivity in children. The incidence of uveitis has decreased because of intensive topical steroids and cycloplegics in the postoperative period.
- Retinal detachments are usually a late complication of pediatric cataract surgery.
- Amblyopia is one of the most important vision-threatening complications. The aphakic or pseudophakic child must be provided with suitable optical correction after surgery. Postoperative patching of the normal eye in cases of unilateral cataracts is done to achieve binocular vision and stereopsis.
Prognosis
Children with congenital cataracts have a good prognosis if treated within the first 2 months of life. Left untreated, the prognosis is poor.
Best Child Doctor for Cataracts in Bangalore
Located in Bangalore, Shekar Eye Hospital is renowned for its exceptional pediatric ophthalmology services, particularly in the treatment of cataracts in children. With a team of highly skilled and experienced child doctors specializing in ophthalmology, Shekar Eye Hospital stands out as a trusted destination for parents seeking the best care for their children. Combining cutting-edge technology with compassionate care, the hospital provides comprehensive evaluations and advanced surgical interventions to address pediatric cataracts. Families can rest assured that their child’s vision is in capable hands at Shekar Eye Hospital, where the focus is always on providing the highest quality care and achieving the best possible outcomes.






